Have you heard of this relatively new treatment technique commonly called "flossing"?
The rise in popularity of floss bands (or compression band therapy, CBT) can be largely due to interest from the Cross Fit world where it is a popular mobility tool for athletes pre competition and training. The idea and frequency of use in a clinical physiotherapy setting post injury or surgery is limited with a lack of good clinical trials currently available. Potentially, common injuries such as sprained ankles, torn muscles and post-operative surgery stiffness can benefit from such techniques.
The proposed benefits include:
- increasing joint range of motion (ROM)
- improved muscle mobility
- decreasing pain levels
- potentially speed up recovery through effect on myofascial release, occlusion and reactive hyperemia
Application
The practical use is generally limited to the joints and muslces of the periphery (the legs and arms for ease of application) though other areas have been "flossed". Stiff joints and/or tight muscles can be the target. Once shown this technique, floss bands can be self-administered as part of a warm up for training and competition to help tissue mobility. The process involves:
- Firmly overlap wrap the floss tape (2.5-7.5cm wide latex rubber band) around the limb (muscle or joint) from proximal to distal (although direction has not been scrutinized)
- Keep on for 2-4 minutes for treatment
- The joint or muscle is moved through active or passive ROM (such as a squat/lunge/calf raise) (Figure 1)
An video example for floss application for a knee can be seen here
note: Neurovascular precautions should be observed during application to avoid numbness, pins and needles or excessive changes to blood flow
Figure 1. Ankle application and ROM
Research
Research into use of floss bands is limited, with scientific explanation of mechanisms and reliable research outcomes generally lacking. Bohlen et al. (2014) examined the effect of knee CBT on blood flow occlusion of the lower leg and found, while there was some improvement in strength, that reactive hyperaemic arterial blood flow showed no change. This would suggest that CBT does not alter blood flow significantly, though quality of this study was poor with a small sample tested (n=5). A search of several databases for clinical studies using floss bands or CBT revealed:
- RCT on shoulder ROM (Kiefer, Lemarr, Enriquez, & Tivener, 2017)
- Case report on Achilles tendinopathy (Borda & Selhorst, 2017)
- Crossover study on ankle ROM and jump performance (Driller & Overmayer, 2017) - 1.8cm improvement in ankle dorsiflexion ROM post application
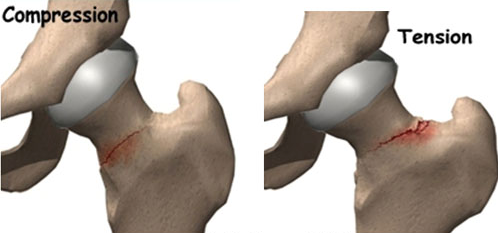
The primary theory of CBT is credited to fascial shearing or re-perfusion of blood to muscle (though as mentioned above the latter is less likely). The role of fascia is varied and can act to restrain motion, as a connective structure for skin or provide lubrication or gliding movement (Guimberteau, Delage, McGrouther, & Wong, 2010). The same group of researchers looked at fascial sliding in the hand during surgery with a visual description seen in Figure 2. Perceivably, with peripheral joints lacking bulky overlying tissue, this sliding of the superficial fascia is possible with CBT but yet to be researched. Another purported mechanism has suggested some psychological benefits following application of CBT to the shoulder (Kiefer et al., 2017).
Figure 2. Three-dimensional model of continuity between the skin and tendon provided by the sliding system (Guimberteau et al., 2010)
Conclusion?
At this stage any conclusions are merely anecdotal. Application of CBT/floss bands can potentially be a useful adjunct to current treatment techniques for acute joint sprain stiffness and restoring ROM. In my experience there seems to be a consistent effectiveness with ankle and knee ROM in the short term. Further review for the effectiveness with knee ROM post-surgery is warranted due to the increased presence of knee stiffness that is often seen. More studies are still needed though to get a better understanding of the proposed mechanisms of floss band treatment.
For more information or to give it a try ask one of your physiotherapists next time you see them!
References
Bohlen, J., Arsenault, M., Deane, B., Miller, P., Guadagno, M., & Dobrosielski, D. A. (2014). Effects of applying floss bands on regional blood flow. International Journal of Exercise Science, Conference Proceedings, 9(2).
Borda, J., & Selhorst, M. (2017). The use of compression tack and flossing along with lacrosse ball massage to treat chronic Achilles tendinopathy in an adolescent athlete: a case report. Journal of Manual & Manipulative Therapy, 25(1), 57-61. doi:10.1080/10669817.2016.1159403
Driller, M. W., & Overmayer, R. G. (2017). The effects of tissue flossing on ankle range of motion and jump performance. Physical Therapy in Sport, 25, 20-24. doi:10.1016/j.ptsp.2016.12.004
Guimberteau, J. C., Delage, J. P., McGrouther, D. A., & Wong, J. K. F. (2010). The microvacuolar system: how connective tissue sliding works. The Journal of hand surgery, European volume, 35(8), 614. doi:10.1177/1753193410374412
Kiefer, B. N., Lemarr, K. E., Enriquez, C. C., & Tivener, K. A. (2017). A Pilot Study: Psychological Effects of the Voodoo Floss Band on Glenohumeral Flexibility. International Journal of Athletic Therapy and Training, 1-16. doi:10.1123/ijatt.2016-0093